What is a Fractured Cusp?
A weakened cusp often leads to a fracture, which could be removed by your dentist, or it might break off on its own. A root canal might be in order, if the pulp ends up damaged, and quite possibly a full crown.A cracked tooth presents itself with various types of symptoms, including pain when chewing, temperature sensitivities, or even discomfort upon the release of biting pressure. It’s also not unusual for the pain to go away, then come back, which makes it harder to diagnose why there is discomfort
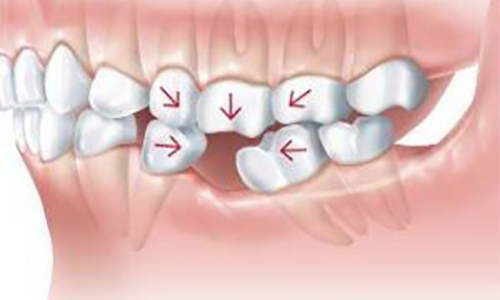
What are the Causes of a cracked tooth?
Teeth crack because of a variety of issues, including:
• pressure from teeth grinding
• fillings so large they weaken the integrity of the tooth
• chewing or biting hard foods, such as ice, nuts, or hard candy
• blows to the mouth, such as might happen with a car accident, sporting injury, fall, or even a fistfight
• abrupt changes in temperature in the mouth — for instance, from eat something extremely hot and then trying to cool your mouth with ice water
• age, with most teeth cracks occurring in people over 50
What are the Treatment Options for Fractured Cusp?
Depending on the severity of the fracture:
• Filing – Part of the tooth can be filed down, if the crack is minor. This will take the edge off and will likely be enough, unless it cracks further for some reason.
• Dental Bonding – The fractured portion of the tooth is bound together, or partial replacement, with a white filling material.
• Crown – If the tooth has a significant crack, the doctor might suggest a crown. This will cover the cracked tooth, protecting it from further cracking.
• Root Canal – If the crack has reached into the pulp, it could affect the nerve, creating intense pain. At this point, it will be recommended you have a root canal performed. The pulp is cleansed, and then filled. Afterward, a crown will be placed on the tooth.